CPT for PEG tube removal delves into the intricacies of the procedure, providing a clear understanding of the medical reasons, assessment criteria, and potential complications associated with PEG tube removal. This comprehensive guide explores the procedure’s nuances, empowering healthcare professionals with the knowledge to make informed decisions.
PEG tube removal, guided by specific CPT codes, is a crucial aspect of patient care. This guide unpacks the complexities of the procedure, providing valuable insights into its indications, techniques, and post-operative management.
CPT Code for PEG Tube Removal
The Current Procedural Terminology (CPT) code assigned to PEG tube removal is 49445.
This code covers the procedure of removing a percutaneous endoscopic gastrostomy (PEG) tube, which is a feeding tube placed directly into the stomach through the abdominal wall.
Procedure Description
The procedure typically involves the following steps:
- The patient is placed in a supine position.
- The skin around the PEG tube is cleansed and draped.
- The PEG tube is grasped with a clamp and pulled out of the stomach.
- The skin incision is closed with sutures or a skin adhesive.
Indications for PEG Tube Removal
PEG tube removal is considered when the underlying medical condition that necessitated its placement has resolved or improved, and the patient can resume adequate oral intake. The decision to remove a PEG tube is made by a healthcare professional, typically a gastroenterologist or surgeon, after a thorough assessment of the patient’s condition.
The assessment criteria used to determine when PEG tube removal is appropriate include:
Medical Conditions Improved
- Resolution of the underlying medical condition, such as stroke, head injury, or esophageal obstruction, that led to the PEG tube placement.
- Improvement in the patient’s neurological status, allowing for safe swallowing and adequate oral intake.
- Healing of esophageal or gastric lesions that previously prevented oral intake.
Nutritional Status
- The patient is maintaining adequate nutritional status without the use of the PEG tube.
- The patient has demonstrated consistent oral intake and weight gain.
- Laboratory tests show normal nutritional parameters.
Patient’s Preference and Goals
- The patient expresses a desire to have the PEG tube removed.
- The patient understands the risks and benefits of PEG tube removal.
- The patient’s goals align with PEG tube removal, such as improved quality of life or reduced dependence on medical devices.
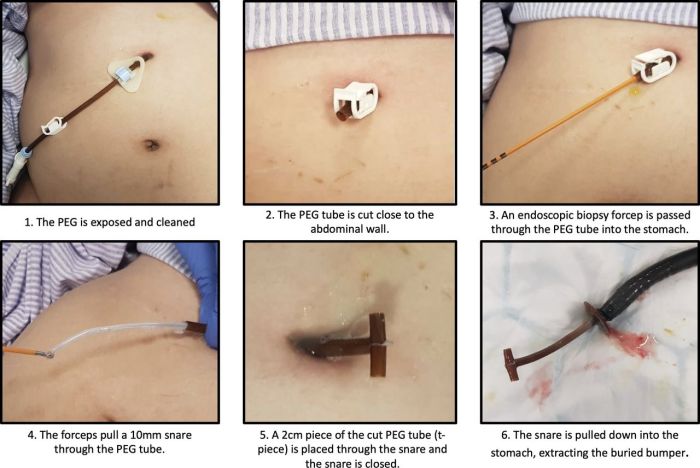
Procedure for PEG Tube Removal
PEG tube removal is a relatively straightforward procedure that can be performed in an outpatient setting. The procedure typically takes about 30 minutes and involves the following steps:
Pre-operative preparation:
- The patient will be asked to fast for 8 hours before the procedure.
- The patient will be given antibiotics to prevent infection.
- The patient will be given a sedative to relax them during the procedure.
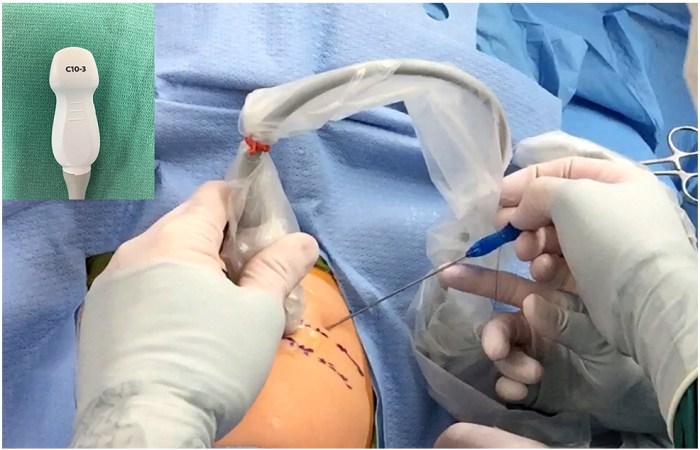
Anesthesia:
The patient will be given local anesthesia to numb the area around the PEG tube. In some cases, the patient may also be given general anesthesia.
CPT for PEG tube removal is a topic covered in detail in unit 7 session 1 letrs . The session provides comprehensive information on the procedure, including indications, contraindications, and potential complications. Understanding CPT for PEG tube removal is crucial for healthcare professionals involved in the management of patients with PEG tubes.
PEG tube removal:
The doctor will use a scalpel to make a small incision around the PEG tube. The doctor will then gently pull the PEG tube out of the stomach. The doctor will then suture the incision closed.
Post-operative care:
- The patient will be monitored for any complications, such as bleeding or infection.
- The patient will be given pain medication to relieve any discomfort.
- The patient will be given instructions on how to care for the incision.
Chronological Procedure Steps
The following table provides a chronological overview of the PEG tube removal procedure:
| Step | Description |
|---|---|
| 1 | Pre-operative preparation |
| 2 | Anesthesia |
| 3 | PEG tube removal |
| 4 | Post-operative care |
Complications of PEG Tube Removal: Cpt For Peg Tube Removal
PEG tube removal is generally a safe procedure, but it can be associated with certain complications. These complications are relatively uncommon but can occur due to various factors, including the patient’s underlying health conditions, the skill of the healthcare provider performing the procedure, and the specific technique used for removal.
It is important for healthcare providers to be aware of the potential complications and take appropriate preventive measures to minimize the risk of their occurrence.
Bleeding
- Risk factors: Coagulopathies, anticoagulant use, excessive traction during tube removal
- Preventive measures: Assess coagulation status, discontinue anticoagulants if possible, use gentle traction during removal
Infection
- Risk factors: Immunosuppression, contaminated equipment, poor wound care
- Preventive measures: Use sterile technique, administer antibiotics if indicated, provide wound care instructions to the patient
Perforation of the gastrointestinal tract
- Risk factors: Adhesions, previous abdominal surgery, excessive force during removal
- Preventive measures: Use caution during removal, especially if there are known adhesions, consider endoscopic guidance if necessary
Granuloma formation, Cpt for peg tube removal
- Risk factors: Excessive inflammation, delayed wound healing
- Preventive measures: Keep the wound clean and dry, apply topical antibiotics or dressings as needed
Patient Education and Follow-Up

Before PEG tube removal, patients must be thoroughly informed about the procedure, its potential complications, and the expected outcomes. They should be educated on the importance of maintaining a healthy diet and lifestyle to prevent the recurrence of conditions that led to the PEG tube placement.
Following PEG tube removal, patients require close follow-up care to monitor for any complications and ensure a successful outcome. This typically involves regular medical appointments, nutritional assessments, and wound care. Patients should be instructed to report any signs or symptoms of infection, bleeding, or pain at the removal site.
Dietary Recommendations
After PEG tube removal, patients should gradually transition to a normal diet. They may initially experience difficulty swallowing or eating due to the absence of the PEG tube, so it is important to start with soft, easily digestible foods. Patients should be encouraged to consume a balanced diet that meets their nutritional needs.
Activity Restrictions
Patients may be advised to avoid strenuous activities or heavy lifting for a period of time after PEG tube removal. This is to prevent undue stress on the removal site and promote proper healing.
Wound Care
The removal site should be kept clean and dry to prevent infection. Patients may be instructed to apply a dressing or ointment to the site and to monitor for any signs of redness, swelling, or drainage.
Follow-Up Appointments
Patients will typically have follow-up appointments with their healthcare provider at regular intervals after PEG tube removal. These appointments allow the provider to assess the patient’s progress, monitor for complications, and provide ongoing support and guidance.
Frequently Asked Questions
What are the indications for PEG tube removal?
PEG tube removal is indicated when the patient no longer requires nutritional support via the PEG tube, or when the tube is causing complications.
What are the steps involved in the PEG tube removal procedure?
The PEG tube removal procedure typically involves deflating the balloon, withdrawing the tube, and closing the stoma site.
What are the potential complications of PEG tube removal?
Potential complications of PEG tube removal include bleeding, infection, and leakage from the stoma site.